Just Published
News

IARC hosts WHO UCN team
The International Agency for Research on Cancer (IARC) hosted senior personnel of the World Healt...
15.04.2024
Read more
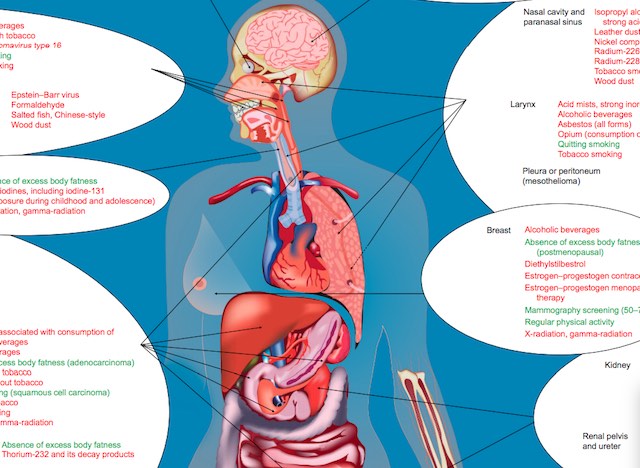
Advisory Group recommendations on priorities for the IARC Monographs
The results of the recent meeting of the Advisory Group to Recommend Priorities for the IARC Mono...
12.04.2024
Read more

IARC Biobank obtains GIS IBiSA label
The biobank of the International Agency for Research on Cancer (IARC) has been granted one of six...
10.04.2024
Read more

IARC and the National Cancer Center of Korea mark 10 years of the HELPER study
Researchers from the International Agency for Research on Cancer (IARC) and the National Cancer C...
09.04.2024
Read more